 |
 |
|
 Dr. Robert D. WeaverDr. Jennifer Zienkowski-ZubelBlog After Wearing Flip-Flops All Summer, Students Head Back to School with Painful Feet Cut Yourself Walking Barefoot? It's More Serious Than You Realize Flip-Flops Tied to Surge in Teenage Heel Pain I've Got This Lump on My Foot-What Could It Be? Foot Pain Ruining Your Golf Swing? Got Gout? Holiday Season Triggers Painful Toes 6 Tips to Protect Your Kids in Fall Sports Soccer Season: Prime Time for Foot and Ankle Injuries Taking a Vacation? Make It Easy on Your Feet Are Your Feet Ready for Spring? Tips for Healthy Feet & Ankles During Winter Sports Is Your Foot Fracture an Early Sign of Osteoporosis? Why does my heel hurt? 
One of the most common questions we are asked by our patients is, "Why does my heel hurt?" While there can be many reasons for heel pain, we categorize heel pain into four major causes: plantar fasciitis, Achilles tendonitis, bursitis and nerve pain. Diagnosing the specific issue depends on the exact location of the pain and how the pain affects the mechanical movement of the leg. The most common cause of the heel pain is plantar fasciitis, which is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. When patients suffer from this ailment, the fascia becomes irritated and then inflamed, resulting in heel pain or pain in the arch of the foot. Plantar fascia pain is a tell-tale sign there are mechanical issues going on in how the foot works. We typically treat plantar fasciitis first with nonsurgical strategies, such as stretching exercises; rest; shoe pads and footwear modifications; orthotic devices; night splints and injection therapy. While most patients respond well to conservative treatments, some require surgery to correct the problem. Achilles tendonitis, or the inflammation of the Achilles tendon, can also be a cause of heel pain. We often see this "overuse" condition in our athletic patients who play high-impact sports, such as basketball or tennis. They often have a sudden increase of repetitive activity involving the Achilles tendon, which puts too much stress on the tendon too quickly, leading to microinjuries of the tendon. To treat Achilles tendonitis, we often immobilize the foot with a walking boot or cast; and also use physical therapy, orthotics and ice to help repair the tendon. If the tendon is severely damaged or if nonsurgical treatments don't work, surgery may be necessary. Another cause of heel pain commonly seen is bursitis, where the "fat pad" of the heel exhibits redness and swelling from inflammation of the small fluid-filled sac inside the heel, called the bursa. The bursa, which protects the heel from friction, can become inflamed from repetitive motion or irritation from shoes. In the case of bursitis, the heel and the toes are most often affected. Treatment may include resting the foot, ice and anti-inflammatory drug therapy, padding and corticosteroid injections to reduce the inflammation and relieve pain. Surgery may be necessary if conservative methods do not provide relief. Finally, a somewhat less common cause of heel pain is nerve pain. When the nerves are involved, it feels more like a burning or electrical pain shooting or radiating down the foot from the heel, typically toward the toes. A patient will often tell me their heel "burns." There are medications that may help with nerve pain, but in this instance, the patient tends to need nerve decompression surgery, a procedure to help "untrap" the nerve causing the pain. Whatever your heel pain, please call our office, 440-442-3113, for proper diagnosis. We are here to help! After Wearing Flip-Flops All Summer, Students Head Back to School with Painful Feet 
The sounds of back to school season include the ringing of school bells and cash registers, the slamming of locker doors, the noisy ruckus of school hallways and cafeterias, and the moans and groans of students over tests, homework and increasingly, their aching feet. Flip-flops are the summer footwear of choice for many students. But while these sandals are inexpensive and stylish, they don’t cushion or support the foot, leading to problems. After wearing flip-flops all summer, some students will head back to school this fall with foot pain and even injuries, therefore, please remember foot pain isn’t normal and can be reduced or eliminated. People may not realize that even into your mid-teens, there’s new bone growing in your heel. Flip-flops don’t cushion the heel, so repetitive stress from walking can inflame that heel bone growth area and cause pain and tenderness. Heel pain and arch pain rank among the most common complaints among students who wear flip-flops. Other flip-flop feet problems students can take back to school include inflammation of the Achilles tendon, painful pinched nerves, sprained ankles, broken or sprained toes, cuts and scrapes, plantar warts, Athlete’s foot, and callus build-up on the heels and toes. Student’s foot pain can be eliminated with simple treatment methods including stretching exercises, ice massage, anti-inflammatory medications and custom or over-the-counter shoe inserts. Back to school season will always be painful for some students, but it doesn’t need to involve foot pain. Please contact our office at 440-442-3113 to have your student’s painful foot evaluated. We are here to help! Cut Yourself Walking Barefoot? It's More Serious Than You Realize 
Bare feet are universally associated with summer, but for those who enjoy walking barefoot, be warned ignoring seemingly minor puncture wounds on the soles of your feet can allow serious infections to develop and spread. Going barefoot heightens the risk for puncture wounds, which require different treatment from cuts because the tiny holes often harbor foreign matter under the skin. Glass, nails, needles and seashells are common offenders. Regardless of the substance, anything that remains in the wound increases your chances for complications. Puncture wounds in the feet too often are superficially treated and is best to get proper care within the first 24 hours to make sure anything that might be embedded in the wound is removed. Research suggests that 10 percent of puncture wounds do result in serious infection, but such complications can be prevented with prompt and appropriate medical attention. The depth and relative cleanliness of a puncture wound are the main factors determining possible infection risk. Studies show 60 percent of patients who required incision and drainage of a puncture wound had something embedded. With the increasing prevalence of drug-resistant bacteria, even healthy people are getting potentially life-threatening staph infections. So if you step on something and the skin is broken, get treated right away. Treatment involves a thorough cleaning to decrease infection risk. Tetanus shots often are needed. Following treatment, the wound should be monitored carefully at home. Sometimes an infection can develop later and migrate to the bones. So if the wound stays red, swollen and sore after a few days, go back to the doctor for further treatment. In all cases, a puncture wound on your foot should never be taken lightly! We are here to help so please given our office a call, 440-442-3113! Flip-Flops Tied to Surge in Teenage Heel Pain 
Many of us are welcoming the warmer weather sporting flip-flop sandals, however, their popularity among teens and young adults is responsible for a growing epidemic of heel pain in this population. We’re seeing more heel pain than ever in patients 15 to 25 years old, a group that usually doesn’t have this problem. A major contributor is wearing flip-flop sandals with paper-thin soles every day to school. Flip-flops have no arch support and can accentuate any abnormal biomechanics in foot motion, and this eventually brings pain and inflammation. Wearing sandals with reasonably strong soles and arch support, especially for girls and young women, might not be considered stylish, but will allow wear sandals for extended periods of time. It is estimated that 15 percent of all adult foot complaints involve plantar fasciitis, the type of heel pain caused by chronic inflammation of the connective tissue extending from the heel bone to the toes. Being overweight and wearing inappropriate footwear are common contributing factors. The pain is most noticeable after getting out of bed in the morning, and it tends to decrease after a few minutes and returns during the day as time on the feet increases. Not all heel pain, however, is caused by plantar fasciitis. It also can occur from inflammation of the Achilles tendon, bursitis, arthritis, gout, stress fractures, or irritation of one or more of the nerves in the region. Therefore, diagnosis by a foot and ankle surgeon to rule out other causes is advised. Initial treatment options for heel pain caused by plantar fasciitis should include anti-inflammatory medications, padding and strapping of the foot and physical therapy. Patients also should stretch their calf muscles regularly, avoid wearing flat shoes and walking barefoot, use over-the-counter arch supports and heel cushions, and limit the frequency of extended physical activities. Most patients with plantar fasciitis respond to non-surgical treatment within six weeks. However, surgery is sometimes necessary to relieve severe, persistent pain. For further information about heel pain, please give our office a call, 440-442-3113, we are here to help! I've Got This Lump on My Foot-What Could It Be? 
As foot and ankle surgeons, we are asked this question quite frequently. We always explain that because bumps on feet can signal both serious and non-serious conditions, it is always best to have all lumps and bumps properly examined by a foot and ankle surgeon. Bumps on feet can vary in size, from that of a pea to the size of a golf ball. They can also vary in location, from the arch of the foot to the ankle area or elsewhere. They may or may not hurt or cause changes in daily activity. But a lump found in the foot has a possibility of being cancerous, and for this reason, must not be ignored. The most common type of lump found in the foot is a soft-tissue mass called a ganglionic cyst. This soft, fluid-filled sac is a benign (noncancerous) bump found on the tendons and joints. A ganglionic cyst can be caused by a leaking of jelly-like fluid from the "capsule" surrounding a joint or tendon and may be located on the top of the foot, near an ankle joint or even on the side of the foot. The cyst will not go away on its own and tends to return, even after being drained. The best way to keep a ganglionic cyst from recurring is to have it surgically removed by a foot and ankle surgeon. Another common type of lump found in feet are plantar fibromas. These often painless, benign masses are fibrous, hard nodules found within the ligament of the foot and are especially common in the arch area on the bottom of the foot. These bumps tend to be less than an inch in diameter but can get larger over time. Nonsurgical treatments, such as steroid injections, physical therapy or orthotic devices, may help relieve any discomfort but will not make the fibroma disappear. Surgery to remove the mass is an option for patients who continue to experience pain following nonsurgical approaches. For foot bumps that are suspected of being cancerous, we perform a biopsy on the area. A tissue sample from the biopsy is then sent to a lab, and advanced imaging or an MRI may be used to gauge more information about the mass. If it is indeed cancer, the foot and ankle surgeon will perform surgery to remove the mass in tandem with an oncologist for cancer treatment. Remember, foot bumps do not tend to go away on their own. The sooner we are able to properly evaluate the bump, the sooner a patient can have peace of mind and move forward with treatment, whether surgical or nonsurgical, so they may resume everyday activity. If you or someone you know has a lump or a bump, please give our office a call for an evaluation, 440-442-3113! Foot Pain Ruining Your Golf Swing? With the Master’s Tournament this weekend, many of you will be itching to get out onto the golf course, therefore, do not let foot pain prevent you from doing so. The barrier to a perfect golf swing could lie in your big toe. Or your heel. Or on the ball of your foot. These are the three areas of your feet most likely to cause pain that can ruin your golf swing. 
Behind these pain-prone spots can lie stiff joints, stretched-out tissues and even nerve damage. But pain relief is possible and frequently does not require surgery. The three most common painful foot conditions that can ruin your golf swing are heel pain, arthritis and pinched nerves.
For the majority of golfers and other patients, simple treatments including custom orthotic devices (shoe inserts), stretching exercises, changes to your shoes, medications, braces, steroid injections and/or physical therapy is warranted. However, if these conservative measures fail to provide adequate relief, surgery may be required. Foot pain is not normal. With the treatment options available, a pain-free golf swing is clearly in view, so please give our office a call, 440-442-3113. Got Gout? Holiday Season Triggers Painful Toes Got gout? If so, we have some recommendations for surviving the holidays: Watch what you eat and drink! Changes in diet, including overindulging in certain foods and beverages, can cause gout attacks this time of year. 
Gout attacks are extremely painful. They are caused when uric acid accumulates in the tissues and/or a joint and crystallizes. This most commonly occurs in the big toe joint. This is because the toe is the coolest part of the body and uric acid is sensitive to temperature changes. Foods that are high in purines contribute to uric acid build-up. If you are prone to gout attacks avoid purine-rich items, such as shellfish (shrimp, crab, etc.), organ meats (kidney, liver, etc.), red meat, red wine and beer. Gout can be treated with medications, diet changes, increasing consumption of appropriate fluids and immobilizing the foot. In some cases surgery is required to remove the uric acid crystals and repair the joint. For more information or if you are experiencing an attack, please give our office, 440-442-3113, a call. We are here to help! 6 Tips to Protect Your Kids in Fall Sports Back-to-school sports season linked to ankle injuries 
If your children are playing sports this fall, pay attention to six tips that could protect them from serious ankle injuries. Every fall, our office notices an increase in ankle injuries among young athletes. Football, soccer and basketball are the sports most likely to lead to sprains, broken bones and other problems. Our top recommendation for parents is to get ankle injuries treated right away. What seems like a sprain is not always a sprain; in addition to cartilage injuries, your son or daughter might have injured other bones in the foot without knowing it. Have a qualified doctor examine the injury. The sooner rehabilitation starts, the sooner we can prevent long-term problems like instability or arthritis, and the sooner your child can get back into competition. Parents should also follow the tips listed below from the American College of Foot and Ankle Surgeons:
Please feel free to contact our office, 440-442-3113, with any questions, concerns and/or to set-up an appointment. For more information on treating ankle sprains, visit the American College of Foot and Ankle Surgeons' patient information web site, FootHealthFacts.org. Soccer Season: Prime Time for Foot and Ankle Injuries Soccer season is in full swing and our practice strongly urges parents and coaches to think twice before coaxing young, injury-prone soccer players to “play through” foot and ankle pain. Skeletally immature kids, starting and stopping and moving side to side on cleats that are little more than moccasins with spikes are a recipe for foot and ankle sprains and worse. Kids will play with lingering, nagging heel pain that, upon testing, turns out to be a stress fracture that neither they, their parents nor their coaches were aware of. By playing with pain, they can’t give their team 100 percent and make their injuries worse, which prolongs their time out of soccer. 
Symptoms of stress fractures include pain during normal activity and when touching the area, and swelling without bruising. Treatment usually involves rest and sometimes casting. Some stress fractures heal poorly and often require surgery, such as a break in the elongated bone near the little toe, known as a Jones fracture. Other types of overuse injuries are Achilles tendonitis and plantar fasciitis (heel pain caused by inflammation of the tissue extending from the heel to the toes). Quick, out-of-nowhere ankle sprains are also common to soccer. Ankle sprains should be evaluated by a physician to assess the extent of the injury. If the ankle stays swollen for days and is painful to walk or even stand on, it could be a fracture. Collisions between soccer players take their toll on toes. When two feet are coming at the ball simultaneously, that ball turns into cement block and goes nowhere. The weakest point in that transaction is usually the foot, with broken toes being the outcome. The toes swell up so much the player can’t get a shoe on, which is a good sign for young athletes and their parents: If they are having trouble just getting a shoe on, they shouldn’t play. For further information about various foot conditions, contact our office, 440-442-3113 or visit FootHealthFacts.org, sponsored by the American College of Foot and Ankle Surgeons. We are here to help and keep your children playing! Taking a Vacation? Make It Easy on Your Feet 
Although rest and relaxation are the goals for most vacations, they usually involve a lot of walking and a lot of walking usually involves sore feet. Walking is great exercise and one of the most reliable forms of transportation, however, if your feet aren’t in the best shape or you don’t have the right shoes, too much walking can cause foot problems.
The right shoe is also important to healthy walking. The ideal walking shoe should be stable from side to side, and well-cushioned, and it should enable you to walk smoothly. Many running shoes will fit the bill. There are also shoes made especially for walking. Walking shoes tend to be slightly less cushioned, yet not as bulky, and lighter than running shoes. Whether a walking or running shoe, the shoes need to feel stable and comfortable. Warming up exercises to help alleviate any muscle stiffness or pulled muscles are also advised before walking. Loosening up the heel cords (Achilles and calf) and thigh muscles before a walk is especially effective. If you’re not accustomed to long walks, start slowly and rest if your feet start hurting, however, above all, have fun!!! Contact our office, 440-840-0616, for more information. We are here to help! Are Your Feet Ready for Spring? 
Its spring, believe it or not! The flowers are about to bloom, the weather will eventually get warmer. All over the country, people are shaking off their winter blues, and getting ready for a season of active outdoor fun. But chances are, not many of them will have feet on their mind– and that may be what puts them on the sidelines when you’re out in the sun! To make sure that you’re not one of the unfortunate souls who has to stay inside this season, we encourage you to follow the tips listed below to prepare your feet for spring: Treat your feet right!Your feet are easy to forget. Especially after a winter of wrapping them in wool socks and heavy boots, it can be hard to remember to take care of them. But this neglect can take its toll: a winter’s worth of wear can lead to dead skin build-up, leading to unsightly calluses and possible corns. Be sure to take care of these with a pumice stone or foot-file, and make sure to wash and dry your feet thoroughly and regularly. Are you moisturizing? You should be! Make sure to stretch!After an entire season without much exercise, it can become clear quickly that your body just isn’t used to moving like it was last Autumn. Jumping into physical activity without proper preparation can lead to some serious issues, like plantar fasciitis and other tendon-based problems. It’s important to build up to your activity peak gradually, and warm up to each new adventure. For a full list of foot-prepping stretches and strength-training exercises, make an appointment with our office. We will help you get on your feet and stay there all summer long. Wear the right shoes!Your feet take a lot of punishment. Without the proper shoes and orthotics, the build-up of damage on your feet and ankles may culminate to something that requires more in-depth treatment. Fortunately, we can help can prescribe the right shoe for the job! We are equipped with the know-how to get you the orthotics you need for the adventures you love. A proper orthotic is invaluable– preventing everything from microfractures to tendon issues and more. If you have any questions about proper springtime footcare, don’t hesitate to give our office a call, we are here to help, 440-442-3113! We have the knowledge and expertise to keep your feet strong this and future seasons! Tips for Healthy Feet & Ankles During Winter Sports From the rush of downhill skiing and snowboarding to cross country skiing to ice skating, cold weather sports provide a fast track for fun and cardiovascular heath, but the colder temperatures and exhilarating speeds attained during such sports can expose your foot and ankles to debilitating injuries. 
Healthy feet and ankles act as accelerators, brakes and shock absorbers in winter sports and help keep the body upright and out of the line of danger. Therefore, avoiding foot/ankle problems is key to full enjoyment during these activities. To ensure an injury–free winter season follow the recommendations listed below:
Follow the tips listed above and enjoy the remainder of this winter season. If you have sustained an injury during a winter sporting activity please give our office a call, 1-440-442-3113, we are here to help! Is Your Foot Fracture an Early Sign of Osteoporosis? Unexplained foot fractures may be the first sign of osteoporosis, a bone thinning disease which affects over 28 million Americans and accounts for 1.5 million bone fractures a year. 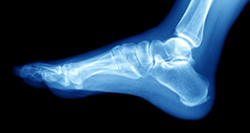
Osteoporosis is frequently referred to as the “silent crippler” since it often progresses without any symptoms or isn’t diagnosed until a person experiences pain from a bone fracture. The porous nature of bones in people with osteoporosis makes them more susceptible to bone fractures, especially in the feet. Because the bones are in a weakened state, normal weight-bearing actions like walking can cause the bones in the foot to break. While osteoporosis is most commonly seen in women over age 50, younger people and men are also affected. Early symptoms can include increased pain with walking accompanied by redness and swelling on the top of the foot. Oftentimes patients don’t seek treatment for their symptoms for weeks or even months, thinking the pain will pass. The best advice is, don’t ignore foot pain of any type. Early intervention can make all the difference in your treatment and recovery.” Diagnose of osteoporosis is made through bone densitometry tests, which measure calcium and mineral levels in the bones through low-dose radiation x-ray, or possibly through a routine x-ray. This is why prevention and early intervention are key; women should make sure bone densitometry tests are part of their wellness examinations when indicated by their physicians. If you are diagnosed with osteoporosis, it’s important to protect your feet from stress fractures. Wear shoes that provide support and cushioning, such as athletic running shoes, to provide extra shock absorption and protection. Custom orthotics may also be recommended to protect the foot from pressure and provide shock absorption, particularly during exercise. If you are suffering from foot pain or suspect you may have osteoporosis, please call our office, 440-442-3113. We are here to help! |
||||||||||||||||
|
Dr. Robert D. Weaver, DPM
|
|||||||||||||||||
